Hospitals play a crucial role in patients’ lives, and effective communication is paramount in ensuring their well-being and satisfaction. From conveying important medical information to addressing concerns and providing support, the way healthcare professionals communicate with patients can impact their overall experience and outcomes significantly. A recent article on 10 Tips for Effective Patient Communication: Improving Satisfaction highlights some best practices that hospitals can adopt to enhance their patient communication strategies.
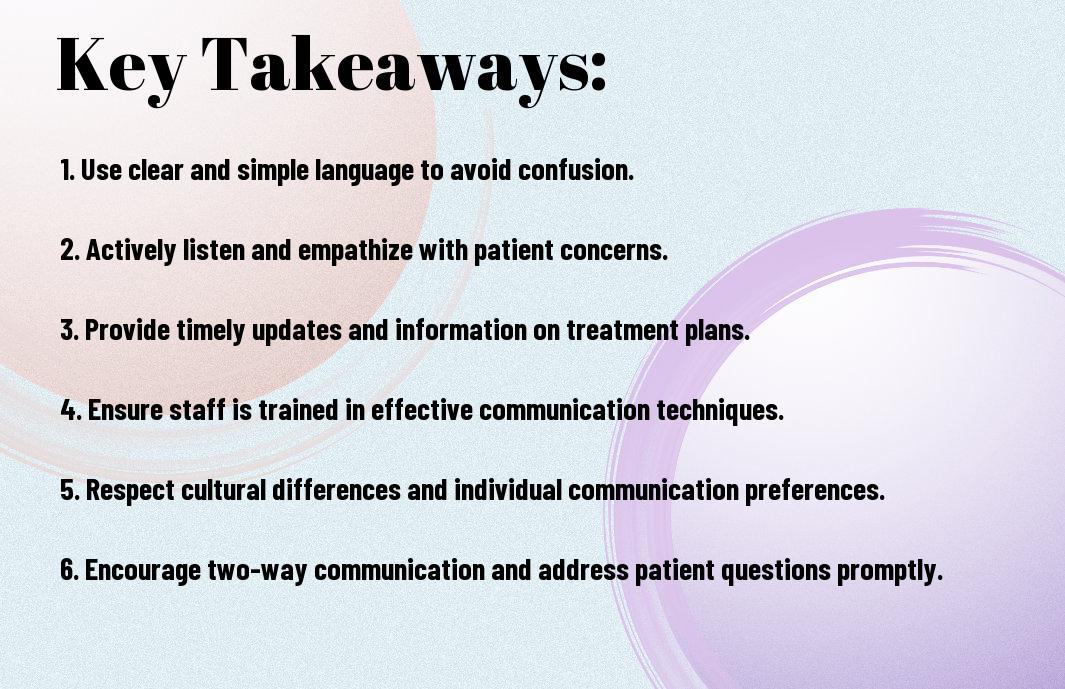
Key Takeaways:
- Active listening: Taking the time to listen to patients without interruption can make them feel valued and understood.
- Clear and simple language: Using jargon-free language when communicating with patients can help prevent misunderstandings and enhance comprehension.
- Empathy and compassion: Showing empathy and compassion towards patients can help build trust and strengthen the patient-provider relationship.
- Non-verbal communication: Paying attention to non-verbal cues such as body language and facial expressions can aid in understanding the patient’s emotions and needs.
- Follow-up communication: Following up with patients after consultations or procedures can help address any additional questions or concerns they may have, leading to improved patient satisfaction.
Understanding Patient Needs
One of the key aspects of effective patient communication in hospitals is understanding the needs of the patients. This involves actively listening to their concerns and assessing their level of understanding regarding their health condition, treatment options, and next steps.
Active Listening Techniques
To engage in effective communication with patients, healthcare providers must practice active listening techniques. This includes giving the patient full attention, maintaining eye contact, and showing empathy towards their feelings. It is crucial to listen not only to the words spoken by the patient but also to their tone of voice and non-verbal cues. Reflecting back what the patient has said can help clarify any misunderstandings and show the patient that their concerns are being heard and validated.
Active listening also involves asking open-ended questions to encourage the patient to share more about their symptoms, concerns, and expectations. By actively listening, healthcare providers can build trust with their patients and establish a strong foundation for effective communication throughout the treatment process.
Assessing Patient Understanding
On top of actively listening to patients, healthcare providers must also assess the patient’s understanding of their health condition and treatment plan. This can be done through techniques such as teach-back, where the patient is asked to explain in their own words what they have understood from the conversation. Assessing patient understanding is necessary to ensure that the patient has comprehended the information provided and can make informed decisions about their healthcare.
The healthcare provider should also use simple and clear language when explaining medical jargon or complex procedures to patients. Ensuring that the patient understands the information presented to them not only improves their compliance with treatment but also enhances their overall healthcare experience.

Communication Strategies
Verbal Communication Skills
For effective patient communication in hospitals, healthcare professionals must develop strong verbal communication skills. Strategies such as using clear and simple language, active listening, and asking open-ended questions can help ensure that patients understand their condition and treatment plan. Additionally, showing empathy and providing reassurance can help build trust and rapport with patients, ultimately leading to better outcomes.
Another key aspect of verbal communication is being aware of non-verbal cues such as tone of voice and body language. Healthcare professionals should maintain a professional yet compassionate demeanor when interacting with patients, as this can greatly influence how the message is received.
Non-Verbal Communication Cues
On top of verbal communication, understanding and utilizing non-verbal communication cues is imperative for effective patient communication. Non-verbal cues such as facial expressions, gestures, and eye contact can convey empathy, understanding, and support without saying a word. Being mindful of these cues can help healthcare professionals connect with patients on a deeper level and establish a sense of trust.
With non-verbal communication playing a significant role in patient interactions, healthcare professionals must pay attention to their own body language and cues they are sending out. Positive non-verbal communication can reinforce verbal messages and create a more supportive and reassuring environment for patients.
Patient-Centered Communication
To effectively communicate with patients in a hospital setting, it is vital to prioritize patient-centered communication. This approach focuses on understanding and meeting the individual needs, preferences, and values of each patient to enhance the quality of care and improve overall patient outcomes.
Building a Therapeutic Relationship
Relationship building is at the core of patient-centered communication. Healthcare professionals should strive to establish a trustworthy and empathetic relationship with their patients based on mutual respect and open communication. Taking the time to listen actively, show compassion, and involve patients in decision-making can foster a sense of partnership and collaboration in the healthcare journey.
Encouraging Patient Involvement in Care
Encouraging Patient Involvement in Care
Communication is key to encouraging patient involvement in their care. Healthcare providers should educate and empower patients to actively participate in decision-making regarding their treatment plans by providing clear and comprehensive information, answering questions, and addressing any concerns. Engaging patients in discussions about their health not only promotes transparency but also helps them feel empowered and in control of their healthcare decisions.
Cultural Competence in Patient Communication
Now, more than ever, cultural competence plays a crucial role in effective patient communication within hospitals. Understanding and respecting the diverse cultural backgrounds of patients is vital for providing high-quality healthcare services.
Recognizing Cultural Differences
The first step in cultural competence is recognizing and acknowledging the cultural differences that exist among patients. These differences can include language, beliefs, values, customs, and communication styles. Being aware of these variations is key to fostering trust and building rapport with patients.
The healthcare staff should undergo training to increase their awareness and understanding of various cultures and how they impact healthcare practices. This training can help them avoid misunderstandings, misinterpretations, and conflicts that may arise due to cultural differences.
Adapting Communication to Meet Cultural Needs
The next critical step in cultural competence is adapting communication strategies to meet the cultural needs of patients. This involves using appropriate language, non-verbal cues, and communication styles that align with the patient’s cultural background.
A healthcare provider should be sensitive to cultural nuances when communicating with patients. This may include using interpreters, respecting personal space preferences, and understanding the significance of eye contact and touch in different cultures. By adapting communication to meet cultural needs, healthcare professionals can enhance patient satisfaction, compliance, and health outcomes.
Communicating with Special Populations
After mastering the vital skills for effective patient communication in hospitals, healthcare providers must also be well-equipped to communicate with special populations. This includes children, elderly patients, and individuals with disabilities. Adapting communication strategies to suit the needs of these diverse groups is crucial in delivering optimal care and building trust.
Strategies for Communicating with Children
Any healthcare professional interacting with children must prioritize building rapport in a non-threatening environment. Using simple, age-appropriate language and engaging them in the conversation can help ease anxiety and foster better understanding. Creating a safe and playful atmosphere can encourage children to express themselves and cooperate during treatments or examinations.
Effective Communication with Elderly Patients
with a growing elderly population, healthcare providers must be equipped to communicate effectively with this group. Patience, empathy, and active listening are key components in ensuring clear and respectful communication with elderly patients. Addressing them by their preferred title, allowing extra time for them to process information, and maintaining eye contact can greatly enhance their overall experience and satisfaction with the care received.
Communication is vital in establishing trust and understanding between healthcare professionals and elderly patients. Miscommunication or lack of clarity can lead to confusion, frustration, and suboptimal care outcomes. By being proactive in improving communication skills and tailoring approaches to individual needs, healthcare providers can ensure a positive and fulfilling healthcare experience for elderly patients.
Tailoring Approaches for Patients with Disabilities
Children and adults with disabilities may require unique communication strategies tailored to their specific needs. Healthcare providers should strive to create a welcoming and inclusive environment, where individuals with disabilities feel respected, understood, and supported. Patience, flexibility, and the willingness to adapt communication methods are paramount in ensuring effective and compassionate care for this population.
Communicating with patients with disabilities may involve the use of alternative communication tools such as visual aids, sign language interpreters, or communication boards. Healthcare providers should always seek to accommodate the individual needs and preferences of patients with disabilities to ensure equitable access to care and promote patient empowerment.
Utilizing Technology for Better Communication
Electronic Health Records and Patient Communication
Your hospital can leverage electronic health records (EHR) systems to enhance communication with patients. By having all patient data centralized and easily accessible, healthcare professionals can provide more personalized care and communicate effectively with patients regarding their treatment plans. EHRs also enable real-time updates on patient progress, allowing for prompt adjustments and better communication between healthcare providers.
Communication through EHRs can also streamline administrative tasks, such as appointment scheduling and prescription refills, making the process more efficient for both patients and healthcare staff. Additionally, patients can access their health information online, empowering them to take an active role in managing their care and fostering a sense of partnership with their healthcare providers.
Telehealth as a Tool for Patient Engagement
With the rise of telehealth, hospitals can now engage with patients remotely, providing access to healthcare services from the comfort of their homes. Telehealth platforms offer features such as video consultations, secure messaging, and remote monitoring, making it convenient for patients to communicate with healthcare providers and receive timely care without the need for in-person visits.
Engagement through telehealth can improve patient outcomes by facilitating regular check-ins, monitoring chronic conditions, and offering educational resources. Patients appreciate the convenience and accessibility of telehealth, leading to higher satisfaction rates and a stronger connection with their healthcare providers.
Also Read: The Importance Of Hospital Safety Measures – Ensuring A Secure Environment For Patients
Summing up
Hence, effective communication with patients is crucial in hospitals to ensure their well-being and satisfaction. By implementing best practices such as active listening, empathy, clear language, and cultural sensitivity, healthcare providers can build trust and rapport with patients, leading to better health outcomes and overall patient experience.
It is vital for hospital staff to continuously improve their communication skills and be mindful of the diverse needs and preferences of patients. By following these best practices, hospitals can create a positive and supportive environment for patients, where they feel heard, understood, and respected throughout their healthcare journey.
FAQs
Q: Why is effective patient communication important in hospitals?
A: Effective patient communication in hospitals is crucial for building trust, improving patient satisfaction, ensuring clarity in treatment plans, and ultimately, enhancing overall patient outcomes.
Q: What are the key components of effective patient communication?
A: Key components of effective patient communication include active listening, empathy, clear and jargon-free language, non-verbal cues, and regular follow-ups.
Q: How can healthcare providers improve their communication skills with patients?
A: Healthcare providers can improve their communication skills by practicing active listening, showing empathy, providing understandable explanations, using open-ended questions, and seeking feedback from patients.
Q: How can hospitals ensure language barriers do not hinder effective patient communication?
A: Hospitals can ensure effective communication despite language barriers by providing professional interpreters, using multilingual staff, utilizing translation services for written materials, and offering cultural competency training to healthcare providers.
Q: What role does body language play in patient communication?
A: Body language plays a significant role in patient communication as it can convey empathy, attentiveness, and understanding. Healthcare providers should be mindful of their body language to create a positive and reassuring environment for patients.
Q: How can hospitals utilize technology to improve patient communication?
A: Hospitals can utilize technology to improve patient communication by implementing electronic health records that are easily accessible to patients, offering telemedicine services for remote consultations, and using secure messaging systems to communicate with patients.
Q: What are some common barriers to effective patient communication in hospitals?
A: Common barriers to effective patient communication in hospitals include time constraints, complex medical jargon, lack of cultural awareness, assumptions about patient understanding, and varying levels of health literacy among patients.